THE ROLE OF DIET IN THE DEVELOPMENT OF CANINE JOINT DISEASE
SEE NO EVIL: Picture a prospective pet owner searching for a new puppy. She wants a bulldog, but she’s unaware that they suffer from a very high incidence of developmental joint diseases. Would it make any difference if she knew the risks? An answer to this question can be found in a series of fascinating experiments in which researchers measured brain activity when people were exposed to health warnings. Specifically, they performed functional brain MRI on smokers exposed to graphic warnings printed on cigarette packages. Most smokers demonstrated no difference in neurological response when they looked at cigarette packets with or without health warnings. In another study, individuals with a responsive brain experienced muted responses after repeated exposures.
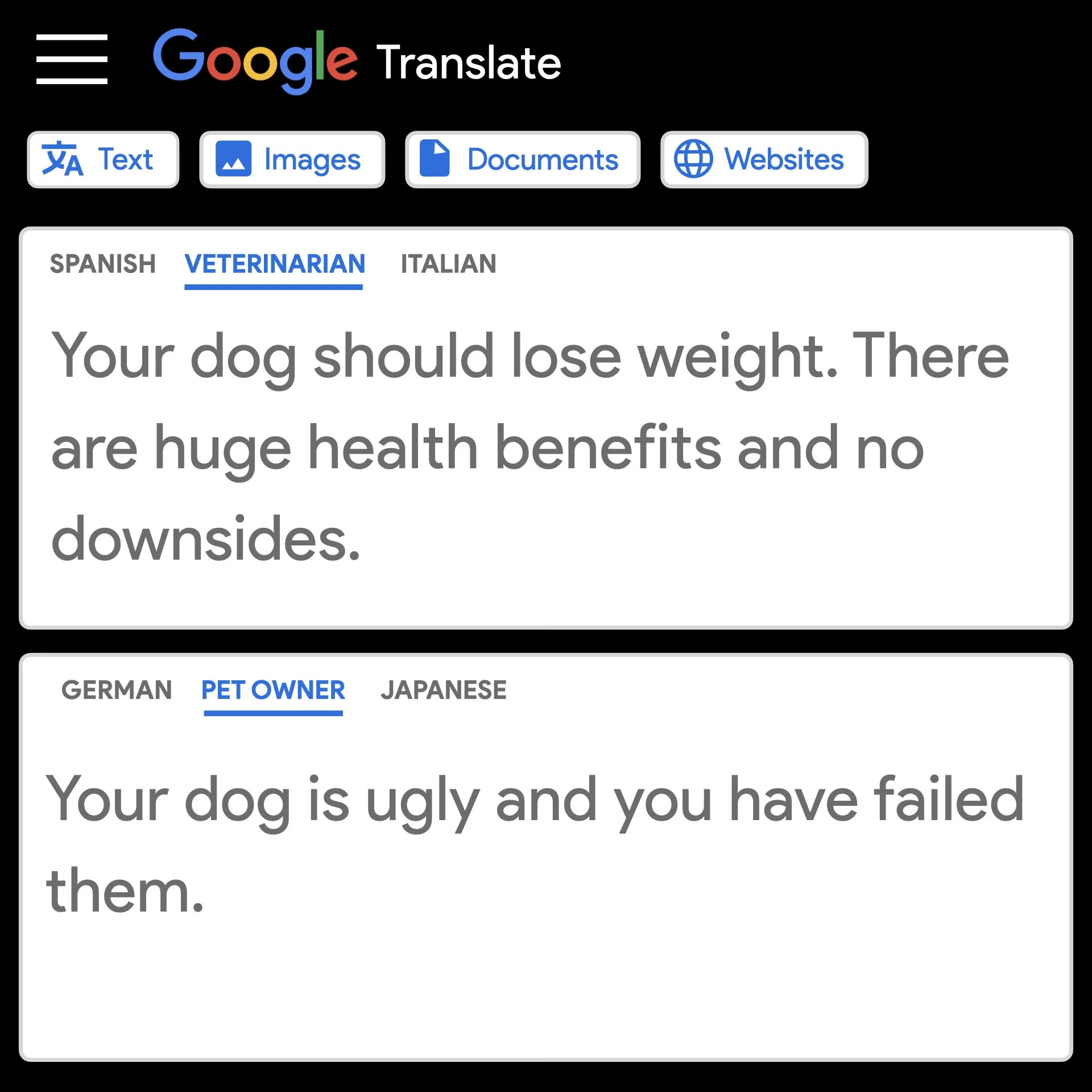
Veterinary studies demonstrate a similar muted response to risk. Despite reporting a high incidence of important breathing difficulties, 7/10 owners of pugs, bulldogs, and French bulldogs rated their dog as very healthy or in the best possible health. Our innate capacity to turn a blind eye to health risks extends to body composition. For instance, one study revealed that 9/10 dog owners understand that being overweight affects the health of their pets, but most continue to overfeed.
CHOOSING A PUPPY: Scene two sees our prospective owner visiting a responsible breeder. Surveying the puppies, she notices their loud breathing. She asks the breeder if her puppies are experiencing breathing difficulties, and learns that bulldogs are prone to a condition called brachycephalic obstructive airway syndrome (BOAS). It’s caused by their squashed faces, narrow nostrils, and elongated palates. The breeder explains that some dogs with BOAS can live happy lives, but others struggle and might require corrective surgery.
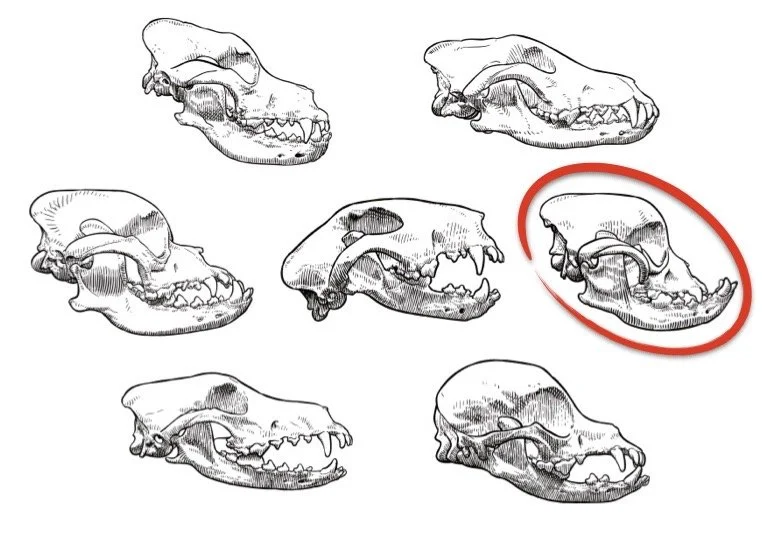
If our prospective owner wants a bulldog, she must learn to live with the consequences of a high-risk conformation. She asks if supplements like glucosamine might help, but she’s informed that no supplement can alter a dog’s anatomy. The responsible breeder patiently explains that a dog’s head and neck conformation are coded into their genes. After taking a few moments to consider this reality, the prospective owner asks, “Is it the same for their joints?”
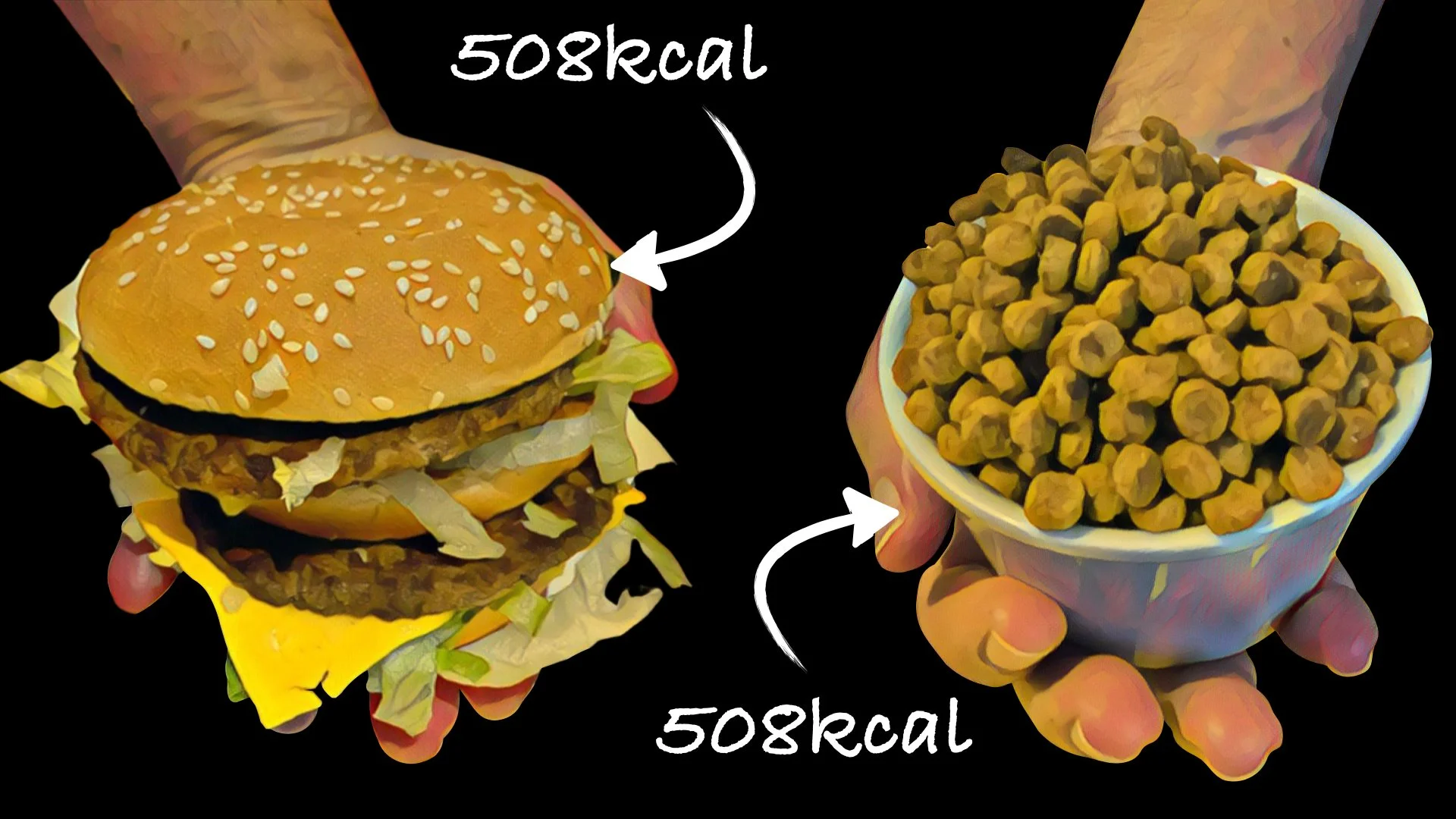
CAN POOR DIET CHOICES CAUSE JOINT DISEASE? In 2008, University of Pennsylvania researchers published the final paper in a series of landmark publications assessing the impact of dietary restriction on canine joint disease. They studied a group of 48 Labrador retrievers recruited from family lines with a high incidence of hip dysplasia. Starting at 8-weeks, 24 puppies ate as much as they wanted, causing them to become overweight.
A second lean-fed group, matched by gender and bodyweight, consumed 25% less than their paired littermates. This group maintained an ideal bodyweight throughout life. The impact of dietary restriction was dramatic. Lean dogs had a five-fold lower risk of hip dysplasia and their overall risk of arthritis was significantly reduced. They developed less severe chronic pain, which occurred relatively later in life.
As a result of calorie restriction alone, lean dogs enjoyed an average lifespan which was 1·8 years longer than their overweight littermates. Critically, the profound health benefits of a low-risk diet had everything to do with excess calories, and nothing to do with the type of food. This isn’t a popular truth for a society which is heavily influenced by pet food branding.
This study isn’t an isolated example of the powerful relationship between overfeeding and joint disease. Another study analysed dogs with cruciate ligament (ACL) injury, which is the commonest cause of chronic hindlimb lameness. Researchers showed that overweight dogs were four-times more likely than lean dogs to injure one or both ACLs. This finding is consistent with many human studies which show a strong link between being overweight and ACL injury.
A vivid illustration of the inflammatory role of adipokines is the proven association between obesity and arthritis in non-weight-bearing joints, including the hand. People don’t walk on their hands, so improvement in hand arthritis after weight loss can only be explained by a biological hypothesis; i.e. a reduction in inflammatory adipokines. Just as arthritis isn’t purely a wear-and-tear phenomenon, body fat isn’t purely an energy depot.
FAT VERSUS CARTILAGE: Until a few years ago, the relationship between overeating and osteoarthritis was thought to be purely mechanical. A biomechanical relationship is intuitive: increased load on joint cartilage causes wear and cartilage breakdown. Less intuitive, and probably more important, is the systemic effect of body fat. Research has shown that body fat is a powerful endocrine organ. It secretes inflammatory chemicals called adipokines, which are found in high concentrations in blood and joint fluid sampled from overweight people with arthritis.
HOW MUCH IS TOO MUCH? In 2021, Washington University researchers performed another landmark study. They bred genetically engineered mice with a condition called lipodystrophy (LD). These mice are unable to deposit body fat even when they’re fed high-fat diets. In other words, they remain lean, no matter what they eat. The research showed knee joints from LD mice were protected from surgically-induced knee arthritis while overweight control mice developed severe pathology. The super-lean LD mice maintained similar pain-thresholds in their surgical and non-surgical knees. In contrast, the control mice, who weighed the same as LD mice but were obese, experienced significantly increased pain responses.
The final striking finding of this study was how little body fat was required to cause harm. Implantation of a surrogate fat pad that restored 20-30% of normal leptin levels (an inflammatory adipokine) reversed the protective effect. This finding reinforced previous research showing systemic inflammation is proportional to the total volume of body fat.
Targeting puppy fat means significantly lowering the risk of painful joint conditions, significantly increasing the probability of a longer, healthier life, and potential lifetime savings averaging US$2000. The importance of a trusting relationship between puppy owners and veterinarians can’t be understated. The ideal way for owners to monitor body composition is a combination of visual inspection and palpation known as body condition scoring (BCS). However, BCS is only validated in adult dogs, and is consistently under-estimated by the general public, even after expert training. In other words, the average dog owner can look at an overweight puppy and see an ideal puppy. Consequently, regular BCS monitoring should be performed by an impartial veterinary professional.
THE CURIOUS CASE OF THE LOW RISK GIANT: The past decade has seen significant press coverage of a proposed link between neutering and joint disease. Particular attention has focused on a 2020 study published in Frontiers in Veterinary Science. The largest breed in this study was a group of 353 great Danes who, despite their rapid growth rate, had no increased risk of joint disease, cancer or urinary incontinence after neutering at any age. This apparent paradox is easily explained. Compared with other breeds, Danes are experts at maintaining lean body mass. In one study, Danes, Labradors and papillons consumed strict calorie-controlled diets. Danes remained leanest as they aged, averaging only 10.5% body fat. Papillons averaged 14.8%, and Labradors topped the charts at 15.7%. This finding supports an indirect relationship between neutering and health problems. In other words, a strong link exists between neutering and obesity, and neutered dogs are nearly three times more likely to be overweight.
WE HAVE A CHOICE: Healthy people shouldn’t move to Mississippi. Alabama, Louisiana, or Tennessee. These US states report obesity rates of 33%, 31%, 30%, and 29%, respectively. All four Southern states differ significantly from neighbouring Colorado, whose residents enjoy a significantly lower risk of obesity, high blood pressure, heart attack, and stroke. The flaw in this argument should be obvious. An individual can choose a healthy lifestyle while living in a high-risk state. Equally, a pet owner can choose to neuter their dog and adjust food intake to maintain a low-risk, lean body mass. The practical problem lies with modern society’s reluctance to accept responsibility. Blaming circumstances rather than ourselves is considered easier than accepting the truth that obesity-related illnesses, including arthritis and cancer, are caused by consuming (or feeding) too many calories.
CAN SUPPLEMENTS COMPETE? Fat-mediated inflammation can be targeted directly using calorie-controlled diets and exercise, or indirectly using anti-inflammatory drugs or supplements. The strongest anti-inflammatory medications are prescription drugs, while the weakest options are supplements including glucosamine, chondroitin, and fish oil. Even so, pet owners often favour joint supplements over fat loss or prescription anti-inflammatory drugs. This behavioural paradox can be explained by a misguided faith in joint supplements. The implausibility and lack of scientific support for a structure-modifying effect of joint supplements doesn’t prevent dog owners believing the hype. People want to believe that supplements can influence the conformation of joints and the structure of cartilage. The fact that it isn’t true appears irrelevant.
WHERE’S THE SCIENTIFIC PROOF? The superiority of fat loss over joint supplements is supported by robust scientific evidence. The most powerful form of medical evidence is a systematic review or meta-analysis of randomised controlled trials (RCTs). In 2018, a meta-analysis of RCTs investigated the effect of two popular supplements, glucosamine and chondroitin sulphate, on knee arthritis symptoms. This powerful study revealed no significant positive effect on self-reported pain measured using the gold-standard Western Ontario and McMaster Universities Osteoarthritis index (WOMAC). A similar systematic review of 30 RCTs evaluating fish oil showed no significant benefit for the treatment of osteoarthritis. In contrast, a meta-analysis of trials evaluating the effect of fat loss on knee arthritis showed that 5-10% weight loss significantly improved pain, disability and quality of life. Sadly, misplaced public faith in joint supplements means powerful treatments like weight loss are rarely prioritised.
HOW TO FIGHT PUPPY FAT: When accurate techniques are used to measure maintenance energy requirement (MER) in pet dogs, significant individual variation is expected. For example, one study identified an individual variation of 32%. In effect, relying exclusively on food package guidelines to determine portion size could result in a 32% error in calorie intake. This profound individual variation is another reason why veterinary BCS measurement is so critical. This is especially important for puppy owners who believe the fallacy that strict exercise restriction is a healthy option. In reality, the benefits of regular exercise aren’t limited to improved core strength, fitness, and social skills. Exercise decreases serum leptin levels, and has a systemic anti-inflammatory effect through cytokines of muscular origin.
Maintenance energy requirements for growing puppies are 2–3 times what would be expected for adult dogs of the same body weight. This ratio considers increased activity as well as growth, and pet food manufacturers factor high activity into their puppy feeding calculations. If owners choose to severely restrict exercise, package guidelines will severely over-estimate ideal calorie intake.
Ultimately, calorie intake and physical activity define a puppy’s body composition. This, in turn, strongly influences a puppy’s risk of joint disease. Consequently, calorie-counting should be used to quantify energy input and accelerometers should be used to quantify energy output.
Professor Stuart Carmichael graduated from the University of Glasgow in 1978. He holds the RCVS diploma in veterinary orthopaedics and is a board-certified specialist. Professor Carmichael was part of the groundbreaking collaborative research team which demonstrated significant improvements in arthritic dogs following a weight loss programme [1].
Mike Farrell graduated from the Royal Veterinary College in 1997. He has over 50 peer-reviewed publications, including papers on the natural history of hip dysplasia, elbow dysplasia, and patellar luxation. Mike holds the ECVS diploma in small animal surgery and is an EBVS and RCVS board-certified specialist.